 Pre-existing condition…
Pre-existing condition…
The pre-existing condition is a health condition or illness that you have had before your first day of coverage on a new plan. The actual health coverage for those with pre-existing conditions depends on a number of factors such as the type of health insurance plan, the level of care that required for your pre-existing condition, and your health insurance history. A person with a pre-existing condition can cost an insurance company big bucks and naturally, it is in their best interest to exclude those who have them.
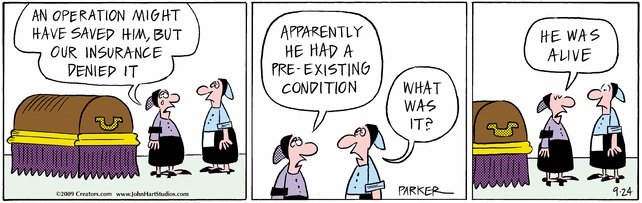
On the ligth side, here’s The Wizzard of ID cartoon that does describe the meaning of pre-existing condition on a morbid way:
 If you don’t like the answer…
If you don’t like the answer…
A significant part of a claim assistance professionals work consists of follow up with insurance companies. We send claims, appeals, and other items, and wait, usually 30 days, to have it processed.
Today I called an insurance company to follow up on a claim submissions as well as two appeals. I was told by the customer service representative that they cannot do anything until the Human Resources department update specific files. I was advised to request this information to be sent to the insurance company directly from the member’s HR Department. Having been doing this for several years, I’ve learned not to argue and didn’t get carried away. After all, this is business as usual….
So, naturally I waited about 10 minutes to simmer over and called again the same insurance company, the same phone number, and naturally about the same claims and appeal letters. The second call yielded a completely different result. The customer service representative checked the claims, verified that all information is correct, and on the file, and promised to reprocess these same claims by the end of this week.
The lesson of my story: if you decide to call your insurance, and push all the necessary buttons on your phone, while lucky enough to get a life human being, the answers aren’t always the same. Therefore, if you don’t like to response, call again and repeat as necessary.
 Health care reform update….
Health care reform update….
With the change of season the health care debate cooled off. The democratic congress created monster health care bill is a thing of a past. The Senate Finance Committee began the markup of Senator Max Baucus’ version of health care reform. This bill promise coverage for more Americans along with controlling cost. The first vote expected by the end of the week.
 Mistakes and confusions…
Mistakes and confusions…
A claim for a diagnostic imaging of a broken bone has been submitted to an insurance company. The claim was denied by the insurance company, citing the lack of reason for medical necessity. One would think that presistenent pain should deserve proper diagnoses and treatment .
In the world of the insurance companies that’s not always the case!
Soon after the denying the claim, an appeal had been filed. The response to the appeal should have been a simple overturn of a denial, but the response was denial of the appeal. Following regular appeals procedure, a second level of appeal had been filed to have the claim paid. That is when things got interesting….
The second level was denied based for the reason of “no first level of appeal on file”. Having the first level of denial in hand, I call the insurance company to say “I have the first level of denial in my hand, where do I fax it?” To my surprise the insurance company isn’t interested on my documentation; they rely on CareCore for information and they are going with that! They need to investigate and will give me a call back. There isn’t a way for me for moving forward, so I wait. A few days later I receive a call back. I am told that the appeal was filed as a “provider appeal”, therefore I have to re-file the first level. At this point I call the billing department of the hospital at 7 AM and to my surprise a billing supervisor picks up the phone. She verifies that the hospital has not filed any appeal.
Just to keep things in motion I re-send all the papers to CareCore. In return I get a call back from a confused nurse, who wants to start an approval process for a new service. No more broken bones please…
By this time, I have made a new friend at the insurance company who is telling me that “this is very frustrating”. You don’t say… Following many more phone calls, it turns out that CareCore, and the radiology management subcontractor made couple of mistakes during the filing process. The entire mess is elevated to management level for correcting the mistake, but unfortunately, it requires more paperwork. After two weeks of trading phone calls, and admission of mistakes, I get to file my second level of appeal for the diagnostic image of a broken bone claim. The insurance company will evaluate the second level of appeal and they’ll let me know within 30 days. By no means the second level of appeal is a slam dunk, it still could be denied for the reason of medical necessity. In that case my new friend at the insurance company will get more calls and be even more frustrated.
Stay tuned for more…